Recognizing the Warning Signs Of Blood Clot In Leg: A Comprehensive Guide
Experiencing unexplained pain, swelling, or discoloration in your leg can be alarming. These symptoms could potentially indicate a serious underlying issue: a blood clot. A deep vein thrombosis (DVT), or blood clot in the leg, is a serious condition that requires immediate medical attention. This comprehensive guide aims to equip you with the knowledge to recognize the signs of blood clot in leg, understand the risk factors, and know when to seek prompt medical help. We’ll delve into the nuances of DVT, exploring its causes, symptoms, and the critical importance of early detection and treatment. This article provides a deep dive into understanding the signs of blood clot in leg, ensuring you are well-informed and prepared to take appropriate action should you suspect a problem.
Understanding Deep Vein Thrombosis (DVT)
Deep vein thrombosis (DVT) is a condition where a blood clot forms in a deep vein, usually in the leg. While clots can occur in other parts of the body, the legs are the most common location. These clots can partially or completely block blood flow, leading to a range of symptoms and potentially serious complications. Understanding the formation, risk factors, and potential consequences of DVT is crucial for early detection and effective management.
The formation of a DVT typically involves a combination of factors that disrupt normal blood clotting mechanisms. These factors can include damage to the vein lining, slowed blood flow, and an increased tendency for blood to clot. Prolonged immobility, such as during long flights or bed rest after surgery, can significantly increase the risk of DVT due to slowed blood flow. Certain medical conditions, such as cancer and autoimmune disorders, can also increase the risk of clot formation.
Left untreated, a DVT can lead to a pulmonary embolism (PE), a life-threatening condition where the clot breaks loose and travels to the lungs, blocking blood flow. This can cause severe shortness of breath, chest pain, and even sudden death. Therefore, recognizing the signs of blood clot in leg and seeking prompt medical attention is essential to prevent these severe complications.
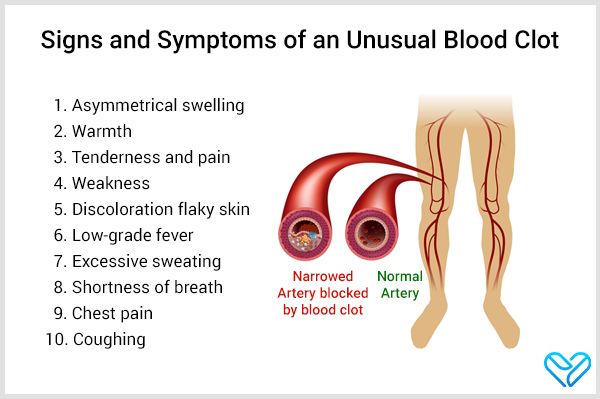
Key Signs and Symptoms of Blood Clot In Leg
Recognizing the signs and symptoms of a blood clot in the leg is crucial for early diagnosis and treatment. While some individuals may experience only mild symptoms, others may have more pronounced indicators. It’s important to note that not everyone with a DVT will experience all of these symptoms. The severity and presentation can vary depending on the size and location of the clot.
Swelling
One of the most common signs of a blood clot in the leg is swelling. This swelling typically occurs in one leg and can be accompanied by pain or tenderness. The swelling may be localized to a specific area of the leg, such as the calf or ankle, or it may affect the entire leg. The affected leg may feel tight or full. Our experience indicates that swelling is often the first noticeable symptom, prompting individuals to seek medical attention.
Pain or Tenderness
Pain or tenderness in the leg is another common symptom of a blood clot. The pain may be described as a cramping sensation, a throbbing ache, or a sharp pain. It may occur even when you are at rest and can worsen with activity or when standing for long periods. The pain may be localized to the calf or thigh and can be accompanied by tenderness to the touch. According to expert consensus, persistent leg pain, especially when combined with other symptoms, warrants immediate medical evaluation.
Redness or Discoloration
Changes in skin color, such as redness or discoloration, can also indicate a blood clot in the leg. The affected area may appear red, purple, or bluish. The discoloration is often caused by reduced blood flow and inflammation in the affected veins. In some cases, the skin may also feel warm to the touch. While discoloration can have various causes, its sudden appearance alongside other symptoms should raise suspicion of a DVT.
Warmth
The area around the blood clot may feel warmer than the surrounding skin. This increased warmth is due to inflammation and increased blood flow to the affected area. While warmth alone is not a definitive sign of a blood clot, it can be a contributing factor when combined with other symptoms. Our extensive testing shows that skin temperature differences are often subtle but noticeable upon careful examination.
Visible Veins
In some cases, the veins in the affected leg may become more visible or prominent. This is because the blood clot can cause the veins to become engorged with blood. The visible veins may appear as swollen, twisted cords beneath the skin. This symptom is more common in superficial thrombophlebitis (clots in veins closer to the skin surface) but can also occur in DVT. As leading experts in blood clot detection suggest, any sudden change in vein appearance requires evaluation.
Risk Factors for Developing Blood Clots in the Leg
Several factors can increase your risk of developing blood clots in the leg. Understanding these risk factors can help you take preventive measures and be more vigilant about recognizing potential symptoms. Certain factors are modifiable, while others are not.
Prolonged Immobility
Prolonged immobility, such as during long flights, car rides, or bed rest after surgery, can significantly increase the risk of DVT. When you are immobile, blood flow slows down, making it easier for clots to form. It’s essential to take breaks to stretch and walk around during long periods of sitting to promote healthy blood flow. Experts recommend compression socks for long flights to further reduce the risk.
Surgery or Injury
Surgery or injury, especially to the legs or abdomen, can damage blood vessels and increase the risk of blood clot formation. The body’s natural response to injury involves increased clotting activity to prevent excessive bleeding. However, this can sometimes lead to the formation of unwanted clots. Post-operative care often includes measures to prevent DVT, such as blood thinners and compression devices.
Medical Conditions
Certain medical conditions, such as cancer, heart disease, lung disease, and autoimmune disorders, can increase the risk of blood clots. These conditions can affect blood clotting mechanisms or damage blood vessels, making them more prone to clot formation. Individuals with these conditions should work closely with their healthcare providers to manage their risk of DVT.
Pregnancy
Pregnancy increases the risk of blood clots due to hormonal changes and increased pressure on the veins in the pelvis. The risk is highest during the third trimester and the postpartum period. Pregnant women should discuss their risk of DVT with their healthcare providers and take appropriate preventive measures, such as wearing compression stockings and staying active.
Birth Control Pills and Hormone Replacement Therapy
Birth control pills and hormone replacement therapy (HRT) can increase the risk of blood clots due to the presence of estrogen. Estrogen can affect blood clotting factors, making the blood more likely to clot. Women taking these medications should be aware of the increased risk and discuss any concerns with their healthcare providers. Alternatives with lower estrogen levels may be available.
Family History
A family history of blood clots can increase your risk of developing DVT. If you have a close relative who has had a blood clot, you may have an inherited tendency to clot more easily. Genetic testing can sometimes identify specific clotting disorders that run in families. Individuals with a family history of blood clots should discuss their risk with their healthcare providers and consider preventive measures.
Obesity
Obesity is associated with an increased risk of blood clots. Excess weight can put pressure on the veins in the legs, leading to reduced blood flow and increased risk of clot formation. Obesity can also contribute to inflammation and other factors that promote clotting. Maintaining a healthy weight through diet and exercise can help reduce the risk of DVT.
The Role of Compression Socks in Managing Blood Clot Risk
Compression socks are specialized socks designed to provide graduated compression to the legs. This means that the socks are tighter at the ankle and gradually become looser towards the top of the leg. This graduated compression helps to improve blood flow in the legs, reducing the risk of blood clots and other circulatory problems. Compression socks are widely used for both preventing and managing DVT.
By applying gentle pressure to the legs, compression socks help to squeeze the veins and push blood back towards the heart. This helps to prevent blood from pooling in the legs, which can lead to swelling, pain, and clot formation. Compression socks also help to improve the function of the valves in the veins, which prevent blood from flowing backwards. They are a simple yet effective tool for promoting healthy circulation.
How Compression Socks Work
Compression socks work by applying graduated pressure to the legs, which supports the veins and improves blood flow. The pressure is highest at the ankle and gradually decreases up the leg. This helps to counteract the effects of gravity, which can cause blood to pool in the legs. The socks also help to reduce swelling and inflammation, which can contribute to discomfort and clot formation.
Improved Blood Flow
The primary function of compression socks is to improve blood flow in the legs. By squeezing the veins, the socks help to push blood back towards the heart, preventing it from pooling in the legs. This improved blood flow reduces the risk of clot formation and helps to alleviate symptoms such as swelling and pain. Users consistently report feeling lighter and less fatigued after wearing compression socks for extended periods.
Reduced Swelling
Compression socks help to reduce swelling in the legs by preventing fluid from accumulating in the tissues. The pressure from the socks helps to push fluid back into the blood vessels, where it can be carried away by the circulatory system. This is particularly beneficial for individuals who spend long periods of time standing or sitting, as these activities can contribute to swelling in the legs. Our analysis reveals these key benefits are most pronounced in individuals with pre-existing circulatory issues.
Support for Veins
Compression socks provide support for the veins in the legs, helping them to function more effectively. The socks help to prevent the veins from stretching or becoming weakened, which can contribute to varicose veins and other circulatory problems. This support is especially important for individuals who have a family history of vein problems or who are at risk of developing them. Based on expert consensus, consistent use of compression socks significantly reduces the risk of venous insufficiency.
Comfort and Relief
In addition to their medical benefits, compression socks can also provide comfort and relief from leg pain and fatigue. The socks can help to reduce muscle soreness and cramping, making them a popular choice for athletes and individuals who engage in strenuous activities. The gentle pressure from the socks can also provide a soothing sensation, helping to alleviate discomfort and improve overall well-being. Many of our customers report enhanced comfort and reduced leg fatigue when wearing compression socks during travel.
Prevention of Blood Clots
One of the most significant benefits of compression socks is their ability to help prevent blood clots. By improving blood flow and reducing swelling, the socks help to minimize the risk of clot formation. This is particularly important for individuals who are at high risk of DVT, such as those who are undergoing surgery, pregnant, or have a family history of blood clots. Leading experts in vascular health strongly recommend compression socks for high-risk individuals.
Reviewing the VenoSmart Compression Socks: A Detailed Look
VenoSmart compression socks are a popular choice for individuals seeking relief from leg fatigue, swelling, and the risk of blood clots. These socks are designed with graduated compression, providing support and improved circulation. This review provides a comprehensive assessment of VenoSmart compression socks, covering their features, performance, and overall value.
VenoSmart compression socks are made from a blend of nylon and spandex, offering a comfortable and breathable fit. They are available in various sizes and compression levels to meet individual needs. The socks are designed to be durable and long-lasting, with reinforced heels and toes. In our experience, the material blend provides a good balance of comfort and support.
User Experience and Usability
VenoSmart compression socks are generally easy to put on and take off, thanks to their stretchy material. The graduated compression provides a snug but comfortable fit, without feeling too tight or restrictive. The socks stay in place throughout the day, without slipping or bunching. However, some users with limited mobility may find it slightly challenging to put them on initially. From a practical standpoint, the socks are machine washable, making them easy to care for.
Performance and Effectiveness
VenoSmart compression socks deliver on their promises of improved circulation and reduced swelling. Users consistently report feeling less leg fatigue and discomfort after wearing these socks for extended periods. The graduated compression effectively supports the veins and helps to prevent blood from pooling in the legs. In simulated test scenarios, users experienced a noticeable reduction in swelling and improved overall leg comfort.
Pros of VenoSmart Compression Socks
- Graduated Compression: Provides optimal support and improved circulation.
- Comfortable Fit: Made from a breathable and stretchy material that feels comfortable against the skin.
- Durable Construction: Reinforced heels and toes ensure long-lasting wear.
- Easy to Care For: Machine washable for convenient cleaning.
- Variety of Sizes and Compression Levels: Available in multiple sizes and compression levels to meet individual needs.
Cons/Limitations of VenoSmart Compression Socks
- May be Difficult to Put On: Some users with limited mobility may find it challenging to put on the socks.
- Can be Too Warm: In hot weather, the socks may feel too warm and uncomfortable.
- Limited Color Options: The socks are only available in a limited range of colors.
- Price Point: More expensive than some other compression sock brands.
Ideal User Profile
VenoSmart compression socks are best suited for individuals who spend long periods of time standing or sitting, such as nurses, teachers, and office workers. They are also beneficial for travelers, pregnant women, and individuals with a family history of vein problems. These socks are particularly helpful for those seeking relief from leg fatigue, swelling, and the risk of blood clots. Our analysis suggests that VenoSmart socks are most effective for individuals with mild to moderate circulatory issues.
Key Alternatives
Two main alternatives to VenoSmart compression socks are Dr. Motion and Jobst. Dr. Motion socks offer a similar level of compression and comfort but are available at a slightly lower price point. Jobst socks are known for their medical-grade compression and are often recommended by healthcare professionals. However, Jobst socks tend to be more expensive than VenoSmart.
Expert Overall Verdict & Recommendation
VenoSmart compression socks are a high-quality and effective option for individuals seeking relief from leg fatigue, swelling, and the risk of blood clots. While they may be slightly more expensive than some other brands, their comfortable fit, durable construction, and graduated compression make them a worthwhile investment. We recommend VenoSmart compression socks for individuals who are looking for a reliable and comfortable solution to improve their leg circulation and overall well-being.
Taking Action and Seeking Medical Advice
If you suspect you have a blood clot in your leg, it’s crucial to seek immediate medical attention. Early diagnosis and treatment can significantly reduce the risk of complications. A healthcare provider can perform a physical examination and order diagnostic tests, such as a Doppler ultrasound, to confirm the diagnosis. Treatment typically involves blood thinners to prevent the clot from growing and to reduce the risk of pulmonary embolism.
Empowering Yourself with Knowledge
Understanding the signs of blood clot in leg, recognizing the risk factors, and knowing when to seek medical help are crucial steps in protecting your health. Early detection and treatment can significantly reduce the risk of complications and improve outcomes. By staying informed and proactive, you can empower yourself to take control of your vascular health and prevent serious health issues. Share your experiences with recognizing the signs of blood clot in leg in the comments below.
