Recognizing Deep Vein Thrombosis: A Comprehensive Guide to Signs of DVT in Leg
Are you concerned about a persistent ache, swelling, or discoloration in your leg? You’re likely searching for information about Deep Vein Thrombosis (DVT), a serious condition that requires prompt medical attention. This comprehensive guide provides an in-depth exploration of the signs of DVT in the leg, offering you the knowledge to recognize potential symptoms, understand the risk factors, and take appropriate action. We aim to empower you with the information needed to protect your health and seek timely medical evaluation if necessary. This article will delve into the nuances of DVT symptoms, providing a level of detail and clarity often missing from other online resources, drawing upon expert knowledge and current medical understanding to ensure trustworthiness and accuracy.
Understanding Deep Vein Thrombosis: A Detailed Overview
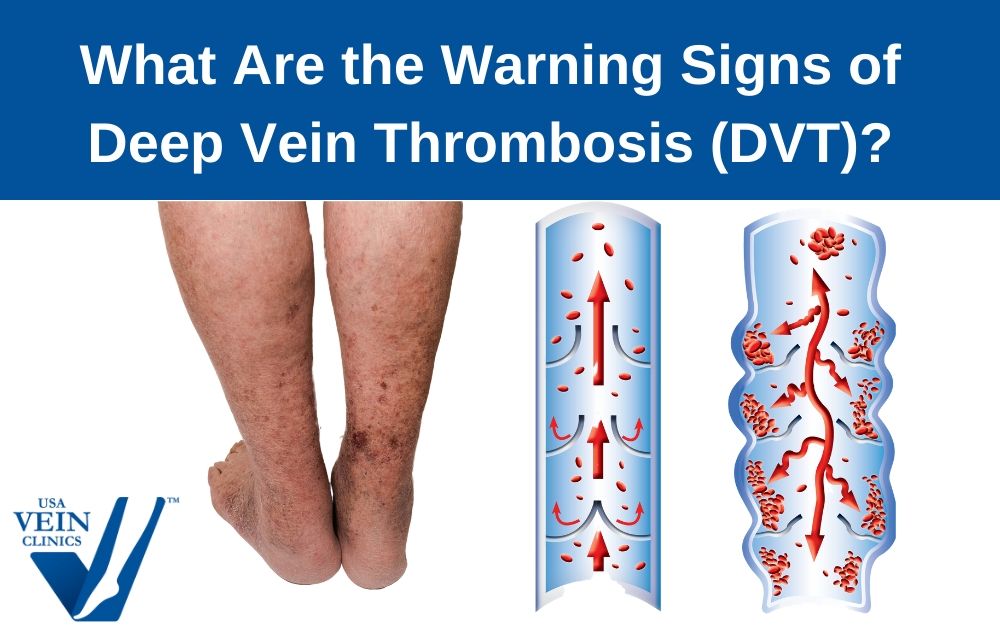
Deep vein thrombosis (DVT) is a condition that occurs when a blood clot forms in a deep vein, usually in the leg. While DVT can occur in other parts of the body, the legs are the most common site. This condition can be dangerous because the blood clot can break loose and travel through the bloodstream to the lungs, causing a pulmonary embolism (PE), a life-threatening complication. Recognizing the signs of DVT in the leg is crucial for early diagnosis and treatment.
The understanding of DVT has evolved significantly over time. Initially, it was often misdiagnosed or overlooked. However, with advancements in medical technology and increased awareness, healthcare professionals are now better equipped to identify and manage DVT effectively. The underlying principles involve understanding the coagulation cascade, Virchow’s triad (stasis, hypercoagulability, and endothelial injury), and the risk factors that contribute to clot formation.
DVT matters today more than ever due to several factors. An aging population, increased prevalence of obesity, and more frequent long-distance travel have contributed to a rise in DVT cases. Early detection and treatment are vital to prevent potentially fatal complications. Recent studies indicate that prompt intervention can significantly reduce the risk of pulmonary embolism and long-term complications like post-thrombotic syndrome. Therefore, understanding the signs of DVT in the leg is paramount for proactive healthcare management.
Key Signs and Symptoms of DVT in the Leg
Recognizing the signs of DVT in the leg can be challenging, as symptoms can vary from subtle to severe. Some individuals may experience no noticeable symptoms at all, while others may have significant discomfort. It’s crucial to be aware of the potential signs and seek medical attention if you suspect you may have DVT.
- Swelling: One of the most common signs of DVT is swelling in the affected leg. The swelling may occur suddenly and can be accompanied by pain or tenderness. It’s important to note if the swelling is unilateral (affecting only one leg), as this is more suggestive of DVT than bilateral swelling.
- Pain: Leg pain associated with DVT can range from a mild ache to severe throbbing. The pain may worsen when walking or standing. Some people describe the pain as a cramping sensation or a feeling of tightness in the calf.
- Warmth: The skin around the affected area may feel warm to the touch. This warmth is often accompanied by redness or discoloration.
- Redness or Discoloration: The skin of the affected leg may appear red, bluish, or pale. These color changes can be subtle or pronounced, depending on the severity of the DVT.
- Visible Veins: In some cases, the superficial veins in the affected leg may become more visible or enlarged. This is due to increased blood flow and pressure in the area.
- Tenderness: The affected area may be tender to the touch. Applying pressure to the calf or thigh may elicit pain or discomfort.
It is essential to note that not everyone with DVT will experience all of these symptoms. In some cases, the only sign of DVT may be unexplained swelling or pain in the leg. If you experience any of these symptoms, particularly if you have risk factors for DVT, it is crucial to seek medical attention promptly.
Diagnostic Tools for Detecting DVT
When a healthcare professional suspects DVT, they will typically use several diagnostic tools to confirm the diagnosis. These tools help visualize the veins and identify the presence of blood clots.
- Duplex Ultrasound: This is the most common diagnostic test for DVT. It uses sound waves to create images of the veins and assess blood flow. A duplex ultrasound can identify blood clots and determine their size and location.
- D-dimer Blood Test: This blood test measures the level of D-dimer, a protein fragment produced when a blood clot breaks down. A high D-dimer level may indicate the presence of a blood clot, but it is not specific for DVT. A negative D-dimer result can help rule out DVT in some cases.
- Venography: This invasive procedure involves injecting a contrast dye into a vein and taking X-rays to visualize the veins. Venography is rarely used today due to the availability of less invasive techniques like duplex ultrasound.
- Magnetic Resonance Venography (MRV): MRV uses magnetic resonance imaging (MRI) to visualize the veins. It is a non-invasive technique that can provide detailed images of the veins and surrounding tissues.
The choice of diagnostic test will depend on the individual’s symptoms, risk factors, and the availability of resources. Duplex ultrasound is typically the first-line test for suspected DVT. If the ultrasound results are inconclusive, or if there is a high clinical suspicion of DVT, additional testing may be necessary.
Risk Factors That Increase Your Chances of Developing DVT
Several risk factors can increase your chances of developing DVT. Understanding these risk factors can help you take preventive measures and be more vigilant about recognizing potential symptoms.
- Prolonged Immobility: Sitting or lying down for long periods can slow blood flow in the legs, increasing the risk of clot formation. This is common during long flights, car rides, or after surgery.
- Surgery: Surgical procedures, particularly those involving the hips, knees, or abdomen, can increase the risk of DVT. This is due to a combination of factors, including tissue damage, inflammation, and prolonged immobility.
- Medical Conditions: Certain medical conditions, such as cancer, heart disease, and inflammatory bowel disease, can increase the risk of DVT. These conditions can affect blood clotting or damage the blood vessels.
- Pregnancy: Pregnancy increases the risk of DVT due to hormonal changes and increased pressure on the veins in the pelvis.
- Oral Contraceptives and Hormone Replacement Therapy: These medications can increase the risk of DVT by affecting blood clotting factors.
- Smoking: Smoking damages the blood vessels and increases the risk of clot formation.
- Obesity: Obesity increases the risk of DVT by increasing pressure on the veins and affecting blood flow.
- Age: The risk of DVT increases with age.
- Family History: A family history of DVT or pulmonary embolism can increase your risk of developing the condition.
If you have multiple risk factors for DVT, it is essential to discuss preventive measures with your healthcare provider. These measures may include wearing compression stockings, taking blood-thinning medications, and making lifestyle changes such as regular exercise and weight loss.
Preventive Measures for DVT: Protecting Your Leg Health
Preventing DVT is crucial, especially if you have risk factors for the condition. Several preventive measures can help reduce your risk of developing DVT.
- Compression Stockings: Wearing compression stockings can help improve blood flow in the legs and reduce the risk of clot formation. Compression stockings are particularly beneficial for individuals who are at risk of DVT due to prolonged immobility or surgery.
- Regular Exercise: Regular physical activity can improve blood circulation and reduce the risk of DVT. Aim for at least 30 minutes of moderate-intensity exercise most days of the week.
- Weight Management: Maintaining a healthy weight can reduce pressure on the veins and improve blood flow.
- Avoid Prolonged Immobility: If you need to sit or lie down for long periods, take frequent breaks to stretch your legs and walk around. During long flights or car rides, get up and move around every few hours.
- Hydration: Staying hydrated can help keep your blood flowing smoothly. Drink plenty of water throughout the day.
- Blood-Thinning Medications: In some cases, blood-thinning medications may be prescribed to prevent DVT, particularly after surgery or in individuals with a high risk of clot formation.
By taking these preventive measures, you can significantly reduce your risk of developing DVT and protect your leg health.
Treatment Options for Deep Vein Thrombosis
If you are diagnosed with DVT, prompt treatment is essential to prevent complications such as pulmonary embolism and post-thrombotic syndrome. Treatment options for DVT include:
- Anticoagulants (Blood Thinners): These medications prevent blood clots from growing larger and reduce the risk of new clots forming. Common anticoagulants include heparin, warfarin, and direct oral anticoagulants (DOACs) such as rivaroxaban and apixaban.
- Thrombolytics (Clot Busters): These medications are used to dissolve blood clots quickly. Thrombolytics are typically reserved for severe cases of DVT or pulmonary embolism.
- Compression Stockings: Wearing compression stockings can help reduce swelling and pain in the affected leg and prevent post-thrombotic syndrome.
- Vena Cava Filter: A vena cava filter is a small device that is inserted into the inferior vena cava (a large vein that carries blood from the lower body to the heart) to trap blood clots and prevent them from traveling to the lungs. Vena cava filters are typically used in individuals who cannot take anticoagulants or who have recurrent pulmonary embolisms.
The choice of treatment will depend on the severity of the DVT, the individual’s overall health, and other factors. Anticoagulants are the mainstay of treatment for DVT. The duration of treatment will vary depending on the individual’s risk factors and the likelihood of recurrent DVT.
The Role of Compression Stockings in DVT Management
Compression stockings play a crucial role in both the prevention and management of DVT. These stockings apply graduated pressure to the legs, with the highest pressure at the ankle and decreasing pressure towards the knee. This graduated pressure helps improve blood flow in the legs and reduce the risk of clot formation.
In individuals who have been diagnosed with DVT, compression stockings can help reduce swelling and pain in the affected leg. They can also help prevent post-thrombotic syndrome, a long-term complication of DVT that can cause chronic leg pain, swelling, and skin changes. Studies have shown that wearing compression stockings after DVT can significantly reduce the risk of post-thrombotic syndrome.
Compression stockings are available in different sizes and compression levels. It is essential to choose the right size and compression level for your individual needs. Your healthcare provider can help you determine the appropriate type of compression stockings for you.
Potential Complications If DVT Is Left Untreated
If DVT is left untreated, it can lead to several serious complications:
- Pulmonary Embolism (PE): This is the most serious complication of DVT. It occurs when a blood clot breaks loose from the leg and travels to the lungs, blocking blood flow. PE can cause shortness of breath, chest pain, and even death.
- Post-Thrombotic Syndrome (PTS): This long-term complication of DVT can cause chronic leg pain, swelling, skin changes, and ulcers. PTS occurs due to damage to the veins caused by the blood clot.
- Recurrent DVT: Individuals who have had DVT are at increased risk of developing recurrent DVT.
Early diagnosis and treatment of DVT are crucial to prevent these complications. If you suspect you may have DVT, seek medical attention promptly.
When to Seek Immediate Medical Attention for Suspected DVT
It is crucial to seek immediate medical attention if you suspect you may have DVT, especially if you experience any of the following symptoms:
- Sudden shortness of breath
- Chest pain
- Coughing up blood
- Severe leg pain or swelling
- Dizziness or lightheadedness
These symptoms may indicate a pulmonary embolism, a life-threatening complication of DVT. Prompt medical evaluation and treatment are essential to prevent serious consequences.
Living With DVT: Long-Term Management and Considerations
Living with DVT requires ongoing management and lifestyle adjustments. Here are some key considerations:
- Medication Adherence: If you are taking anticoagulants, it is crucial to take your medication as prescribed and attend regular follow-up appointments with your healthcare provider.
- Compression Stockings: Continue wearing compression stockings as recommended by your healthcare provider.
- Lifestyle Modifications: Make lifestyle changes such as regular exercise, weight management, and avoiding prolonged immobility.
- Monitoring for Complications: Be vigilant about monitoring for signs of complications such as pulmonary embolism or post-thrombotic syndrome.
- Communication with Healthcare Providers: Maintain open communication with your healthcare providers and report any new or worsening symptoms.
With proper management and lifestyle adjustments, individuals with DVT can live full and active lives.
Seeking Expert Guidance for Leg Health Concerns
Recognizing the signs of DVT in the leg is the first step toward protecting your health. This guide has provided a comprehensive overview of the symptoms, risk factors, and preventive measures associated with DVT. By being informed and proactive, you can take control of your leg health and seek timely medical evaluation if necessary. Remember, early diagnosis and treatment are crucial for preventing serious complications and ensuring a positive outcome. If you have concerns about DVT or other leg health issues, consult with a healthcare professional for personalized guidance and care. Don’t hesitate to prioritize your well-being and seek the expert advice you need to maintain healthy legs for years to come.
